CANCER DIGEST – Dec. 11, 2021 – Using a modified monoclonal antibody in combination with immunotherapy, chemotherapy, radiation therapy and stem cell transplantation, improved survival by 20 percent in children with high-risk neuroblastoma, results of a small clinical trial show.
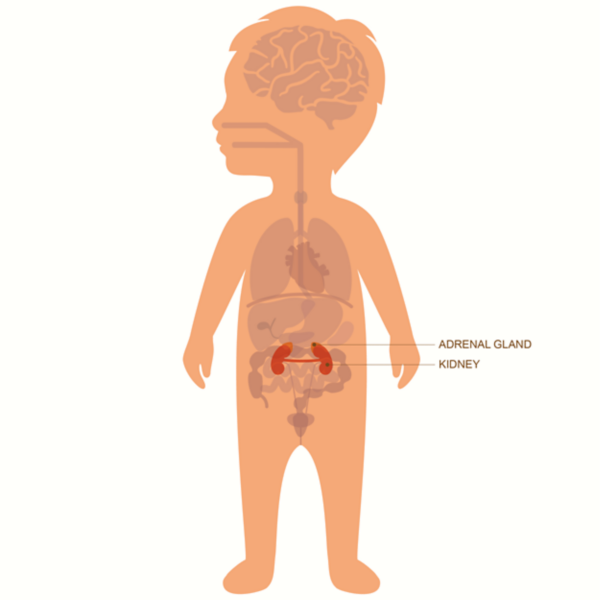
Neuroblastoma is a rare cancer of immature nerve cells and is diagnosed in about 700 people, mostly children under age 5, in the U.S. each year according to the American Cancer Society.
The phase 2 clinical trial, designed to test safety and determine optimal dose, involved 64 patients who received the monoclonal antibody modified by researchers at St. Jude’s Children’s Hospital along with six cycles of chemotherapy and immunotherapy and continuous infusions of pain drugs. Results were published in the Dec. 6, 2021 Journal of Clinical Oncology.
After the first two cycles, 42 patients had their tumor volumes decrease by a median of 75 percent. After three years of follow-up, 73.7 percent survived without disease related events, and overall 3-year survival was 86 percent. Time will tell whether overall 5-year survival is better than the current 40 percent.
“I have treated high-risk neuroblastoma for 30 years, and I have never seen results like this in high-risk patients,” said the study's first author, Wayne Furman, M.D., of St. Jude’s Department of Oncology. “This is the best result published to date for patients with high-risk neuroblastoma, period.”
The monoclonal antibody used was based on a similar one that has been FDA approved, but has shown modest success due to dose limitations because of the pain involved in treating nerve cancer. St. Jude’s researchers modified the monoclonal antibody to reduce dose-limiting pain and other side effects.
If the findings are confirmed in a larger, multi-center trial this new combination could become a standard treatment for these high-risk patients the authors wrote.
Sources: St. Jude Children’s Research Hospital press release and the Journal of Clinical Oncology.
Subscribe to:
Post Comments (Atom)


No comments:
Post a Comment